(→Introduction) |
SunburstTan (Talk | contribs) m (→References) |
||
| (28 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
| − | = | + | <p style=" text-align:top; "> |
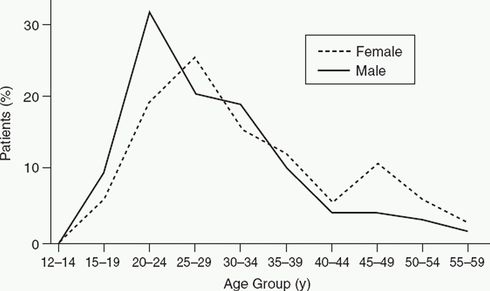
| − | + | [[File:Schizophrenia.jpg|thumb|490px|top| Age of onset of schizophrenia]] | |
| − | + | </p> | |
| − | + | ==Introduction== | |
| + | '''Schizophrenia''' as a whole is beyond the scope of this article. This article is primarily concerned with childhood-onset schizophrenia. | ||
| − | == | + | ===Definitions=== |
| + | * Schizophrenia with onset before age 18 is termed '''early-onset schizophrenia''' | ||
| + | * Onset before age 13 is described as '''childhood-onset schizophrenia''' (COS) | ||
| − | + | ==Epidemiology== | |
| − | + | * The worldwide prevalence of schizophrenia is ~1%, with slight male predominance of approximately '''1.4 to 1'''. | |
| + | *Peak onset of schizophrenia is before age 25 in males, and somewhat later in females, with a second peak in women aged >45. (see figure) | ||
| + | * 25% will recover fully; 4-13% commit suicide. | ||
| + | * COS is rare with rates of 1 per 10,000 (schizophrenia as a whole is 1 per 100). | ||
| + | ===Prognostic factors=== | ||
* Patients whose disease is of acute onset (25%), with productive schizophrenic manifestations such as hallucinations and delusions (positive manifestations), have a better prognosis than those whose disease begins insidiously (75%) and takes an unfavorable course, with depressive states and continually worsening impairment of cognitive function. | * Patients whose disease is of acute onset (25%), with productive schizophrenic manifestations such as hallucinations and delusions (positive manifestations), have a better prognosis than those whose disease begins insidiously (75%) and takes an unfavorable course, with depressive states and continually worsening impairment of cognitive function. | ||
| Line 15: | Line 22: | ||
* The prognosis seems to be better for patients who have no family history of schizophrenia, those whose families cooperate well, and those whose condition improves rapidly during inpatient treatment. | * The prognosis seems to be better for patients who have no family history of schizophrenia, those whose families cooperate well, and those whose condition improves rapidly during inpatient treatment. | ||
| − | * Visual hallucinations are common are correlate with earlier onset, lower IQ and greater clinical impairment as compared to schizophrenic children without visual hallucinations. (David CN. JAACAP 2011) | + | * '''Visual hallucinations''' are common are correlate with earlier onset, lower IQ and greater clinical impairment as compared to schizophrenic children without visual hallucinations. (David CN. JAACAP 2011) |
| − | * The | + | * The most common comorbidity in COS is depression (54%), followed by OCD (21%), GAD and ADHD (15% each) (NIMH) |
* A 42-year longitudinal study of patients with childhood-onset schizophrenia revealed their suicide rate to be higher than that of patients with adult-onset schizophrenia. | * A 42-year longitudinal study of patients with childhood-onset schizophrenia revealed their suicide rate to be higher than that of patients with adult-onset schizophrenia. | ||
| + | ==Diagnosis== | ||
| + | Most often COS is persistent, non-episodic illness with poor prognosis. DSM-5 criteria can be applied to children and adolescents. It's important to rule out affective disorders, substance-induced psychosis as well as autism and PDD. Youth diagnosed with PTSD, conduct problems, depression, and those with history of abuse | ||
| + | report higher rates of psychotic-like symptoms (McClellan JAACAP 2013). | ||
| + | * '''In preschoolers, psychosis (particularly hallucinations) are most likely caused by stress or anxiety'''; these are transient and benign. | ||
| + | * In school-age children, psychotic symptoms may be more persistent, and are more likely to be associated with drug toxicity or significant mental illness (Lewis, p. 494) | ||
| + | * Prescription medications that are associated with psychosis include corticosteroids, anesthetics, anticholinergics, antihistamines, and amphetamines. | ||
| − | === | + | ===Imaging=== |
| − | + | * Youth with EOS exhibit significant '''decreases in gray matter and hippocampal volume reduction''' as well as '''enlargement of ventricular volumes''' compared to normal controls (Steen RG. meta-analysis, BrJPsych 2006); | |
| + | * They also exhibit decreased cortical folding (McClellan J. JAACAP 2013). | ||
| + | ==Treatment== | ||
| + | Atypical antipsychotics are the mainstay of treatment in youth with schizophrenia. (McClellan J. JAACAP 2013) | ||
| + | * Risperidone, aripiprazole, quetiapine, paliperidone, and olanzapine are approved by the FDA dor schizophrenia in adolescents >=13 years based on effecacy in RCTs. | ||
| + | * Ziprasidone RCT was stopped due to lack of efficacy. | ||
| + | * In the only RCT of '''clozapine''', it showed somewhat better results vs olanzapine (particularly in improving negative symptoms), but also more side effects. In the open-label follow-up most children were switched from olanzapine to clozapine. (2) | ||
| + | ===TEOSS Trial=== | ||
In treatment of '''early-onset schizophrenia spectrum disorders (TEOSS) study''', (n=116), first- and second-generation antipsychotics were compared in 8-19 year-olds. Efficasy of risperidone, olanzapine, and molidone (10-140 mg/day) was comparable, but SGA's caused significant weight gain, and olanzapine was associated with hyperlipidemia. (5) | In treatment of '''early-onset schizophrenia spectrum disorders (TEOSS) study''', (n=116), first- and second-generation antipsychotics were compared in 8-19 year-olds. Efficasy of risperidone, olanzapine, and molidone (10-140 mg/day) was comparable, but SGA's caused significant weight gain, and olanzapine was associated with hyperlipidemia. (5) | ||
| + | * Across all three treatments, >50% failed to achieve adequate response after 8 weeks. | ||
| + | |||
| + | Risk of relapse is significant, and antipsychotic maintenance treatment should be continued in most youth with schizophrenia to improve functioning and prevent relapse. (McClellan J. JAACAP 2013) | ||
==Other Pearls== | ==Other Pearls== | ||
| − | |||
| − | |||
*Visual hallucinations are common in COS, and are associated with greater clinical impairment and greater compromise in overall brain functioning. (3) | *Visual hallucinations are common in COS, and are associated with greater clinical impairment and greater compromise in overall brain functioning. (3) | ||
* On imaging, COS children show progressive '''loss of gray matter''' during adolescence (this is not found in adult schizophrenics) | * On imaging, COS children show progressive '''loss of gray matter''' during adolescence (this is not found in adult schizophrenics) | ||
| − | * | + | * [[Omega-3 fatty acids|'''Omega-3 fatty acids''']] can delay the onset of psychosis in high-risk patients. |
| − | + | * NIMH identified a heterogeneous group of children with transient psychotic symptoms and multiple developmental abnormalities had been termed the '''Multi Dimensionally Impaired''' (MDI) group. | |
| − | + | ** These children have cognitive deficits, psychotic symptoms in response to stress without a thought disorder, impaired interpersonal skills, ADHD symptoms, and emotional dysregulation. | |
| − | * | + | ** They are at risk for developing '''bipolar disorder''' later in life. [6] |
* For children on clozapine who develop neutropenia, lithium can be added for clozapine rechallenge [2cases:(4)] | * For children on clozapine who develop neutropenia, lithium can be added for clozapine rechallenge [2cases:(4)] | ||
| Line 50: | Line 71: | ||
5. Sikich, L., Frazier JA. et.al.: Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizo-affective disorder: findings from the treatment of early-onset schizophrenia spectrum disorders (TEOSS) study. Am J Psychiatry. 2008 Nov;165(11):1420-31. | 5. Sikich, L., Frazier JA. et.al.: Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizo-affective disorder: findings from the treatment of early-onset schizophrenia spectrum disorders (TEOSS) study. Am J Psychiatry. 2008 Nov;165(11):1420-31. | ||
| − | {{ | + | 6. Nicolson R, Lenane M, Brookner F, et al. Children and adolescents with psychotic disorder not otherwise specified: a 2- to 8-year follow-up study. Compr Psychiatry. 2001;42:319-325. |
| + | |||
| + | 7. Jon McClellan, M.D., Saundra Stock, M.D., AND AACAP Committee on Quality Issues. Practice Parameter for the Assessment and Treatment of Children and Adolescents With | ||
| + | Schizophrenia. JAACAP, 2013;52(9):976–990 | ||
| + | |||
| + | {{Completeness}} | ||
[[Category:Disorders]] | [[Category:Disorders]] | ||
Latest revision as of 01:30, 7 September 2015
Contents
Introduction
Schizophrenia as a whole is beyond the scope of this article. This article is primarily concerned with childhood-onset schizophrenia.
Definitions
- Schizophrenia with onset before age 18 is termed early-onset schizophrenia
- Onset before age 13 is described as childhood-onset schizophrenia (COS)
Epidemiology
- The worldwide prevalence of schizophrenia is ~1%, with slight male predominance of approximately 1.4 to 1.
- Peak onset of schizophrenia is before age 25 in males, and somewhat later in females, with a second peak in women aged >45. (see figure)
- 25% will recover fully; 4-13% commit suicide.
- COS is rare with rates of 1 per 10,000 (schizophrenia as a whole is 1 per 100).
Prognostic factors
- Patients whose disease is of acute onset (25%), with productive schizophrenic manifestations such as hallucinations and delusions (positive manifestations), have a better prognosis than those whose disease begins insidiously (75%) and takes an unfavorable course, with depressive states and continually worsening impairment of cognitive function.
- The patient's premorbid personality plays a major role. Patients who were described as socially active, intelligent, and integrated children and adolescents before they became ill have a better prognosis than those who were intellectually impaired, timid, introverted and uncommunicative before they became ill. (1)
- The prognosis seems to be better for patients who have no family history of schizophrenia, those whose families cooperate well, and those whose condition improves rapidly during inpatient treatment.
- Visual hallucinations are common are correlate with earlier onset, lower IQ and greater clinical impairment as compared to schizophrenic children without visual hallucinations. (David CN. JAACAP 2011)
- The most common comorbidity in COS is depression (54%), followed by OCD (21%), GAD and ADHD (15% each) (NIMH)
- A 42-year longitudinal study of patients with childhood-onset schizophrenia revealed their suicide rate to be higher than that of patients with adult-onset schizophrenia.
Diagnosis
Most often COS is persistent, non-episodic illness with poor prognosis. DSM-5 criteria can be applied to children and adolescents. It's important to rule out affective disorders, substance-induced psychosis as well as autism and PDD. Youth diagnosed with PTSD, conduct problems, depression, and those with history of abuse report higher rates of psychotic-like symptoms (McClellan JAACAP 2013).
- In preschoolers, psychosis (particularly hallucinations) are most likely caused by stress or anxiety; these are transient and benign.
- In school-age children, psychotic symptoms may be more persistent, and are more likely to be associated with drug toxicity or significant mental illness (Lewis, p. 494)
- Prescription medications that are associated with psychosis include corticosteroids, anesthetics, anticholinergics, antihistamines, and amphetamines.
Imaging
- Youth with EOS exhibit significant decreases in gray matter and hippocampal volume reduction as well as enlargement of ventricular volumes compared to normal controls (Steen RG. meta-analysis, BrJPsych 2006);
- They also exhibit decreased cortical folding (McClellan J. JAACAP 2013).
Treatment
Atypical antipsychotics are the mainstay of treatment in youth with schizophrenia. (McClellan J. JAACAP 2013)
- Risperidone, aripiprazole, quetiapine, paliperidone, and olanzapine are approved by the FDA dor schizophrenia in adolescents >=13 years based on effecacy in RCTs.
- Ziprasidone RCT was stopped due to lack of efficacy.
- In the only RCT of clozapine, it showed somewhat better results vs olanzapine (particularly in improving negative symptoms), but also more side effects. In the open-label follow-up most children were switched from olanzapine to clozapine. (2)
TEOSS Trial
In treatment of early-onset schizophrenia spectrum disorders (TEOSS) study, (n=116), first- and second-generation antipsychotics were compared in 8-19 year-olds. Efficasy of risperidone, olanzapine, and molidone (10-140 mg/day) was comparable, but SGA's caused significant weight gain, and olanzapine was associated with hyperlipidemia. (5)
- Across all three treatments, >50% failed to achieve adequate response after 8 weeks.
Risk of relapse is significant, and antipsychotic maintenance treatment should be continued in most youth with schizophrenia to improve functioning and prevent relapse. (McClellan J. JAACAP 2013)
Other Pearls
- Visual hallucinations are common in COS, and are associated with greater clinical impairment and greater compromise in overall brain functioning. (3)
- On imaging, COS children show progressive loss of gray matter during adolescence (this is not found in adult schizophrenics)
- Omega-3 fatty acids can delay the onset of psychosis in high-risk patients.
- NIMH identified a heterogeneous group of children with transient psychotic symptoms and multiple developmental abnormalities had been termed the Multi Dimensionally Impaired (MDI) group.
- These children have cognitive deficits, psychotic symptoms in response to stress without a thought disorder, impaired interpersonal skills, ADHD symptoms, and emotional dysregulation.
- They are at risk for developing bipolar disorder later in life. [6]
- For children on clozapine who develop neutropenia, lithium can be added for clozapine rechallenge [2cases:(4)]
References
1. Neuropsychobiology 2012;66(1):63-9 "Early-onset schizophrenia"
2. Shaw P et.al Childhood-onset schizophrenia: A double-blind, randomized clozapine-olanzapine comparison. Arch Gen Psychiatry. 2006 Jul;63(7):721-30.
3. David Cn et. al. Childhood onset schizophrenia: high rate of visual hallucinations.J Am Acad Child Adolesc Psychiatry. 2011 Jul;50(7):681-686.e3. Epub 2011 Jun 11.
4. Sporn A, et al.: Clozapine-induced neutropenia in children: Management with lithium carbonate. J Child Adolesc Psychopharmacol 13(3):401–404, 2003
5. Sikich, L., Frazier JA. et.al.: Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizo-affective disorder: findings from the treatment of early-onset schizophrenia spectrum disorders (TEOSS) study. Am J Psychiatry. 2008 Nov;165(11):1420-31.
6. Nicolson R, Lenane M, Brookner F, et al. Children and adolescents with psychotic disorder not otherwise specified: a 2- to 8-year follow-up study. Compr Psychiatry. 2001;42:319-325.
7. Jon McClellan, M.D., Saundra Stock, M.D., AND AACAP Committee on Quality Issues. Practice Parameter for the Assessment and Treatment of Children and Adolescents With Schizophrenia. JAACAP, 2013;52(9):976–990
|
Article Progress | |||||||||
| Write | Edit | Finalize | |||||||
Content |
Completeness | Index Links | Trial Release | Final Check | |||||
.